News & Promotions
 For over 40 years the standard surgical treatment for glaucoma was a procedure called a trabeculectomy.In a trabeculect...
For over 40 years the standard surgical treatment for glaucoma was a procedure called a trabeculectomy.In a trabeculect...
Featured Monthly Video
- Written by InnovativEyes
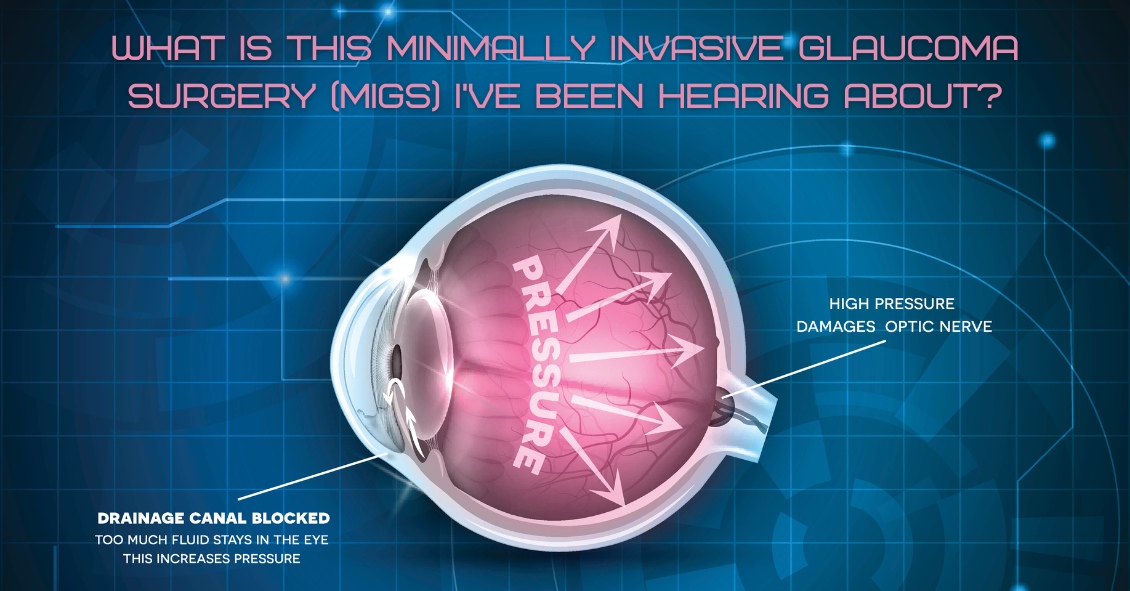
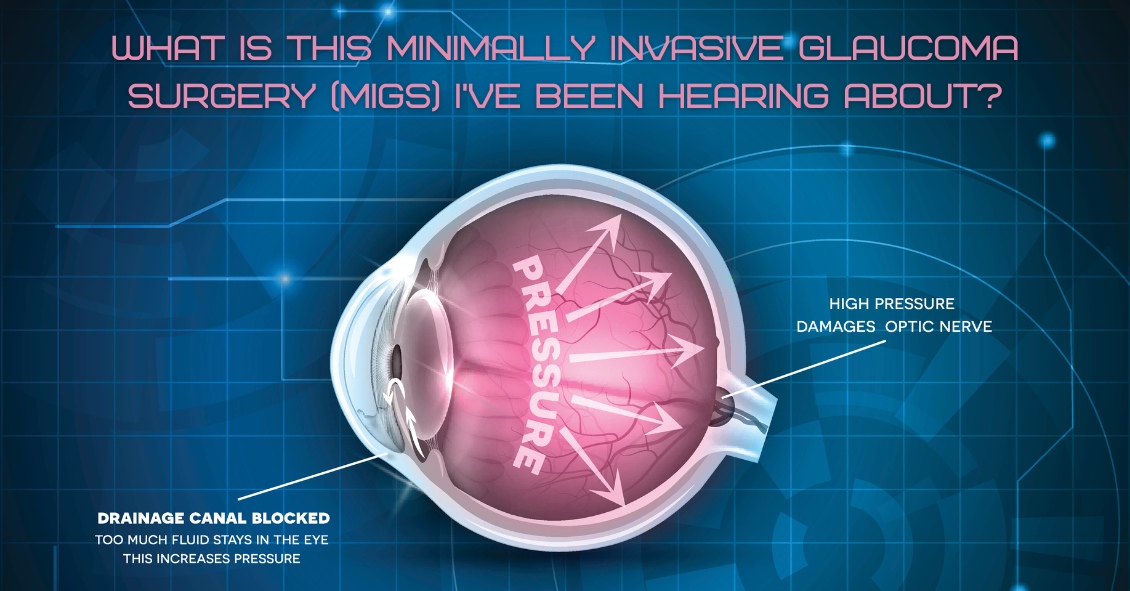
For over 40 years the standard surgical treatment for glaucoma was a procedure called a trabeculectomy.
In a trabeculectomy, the ophthalmic surgeon would make a hole in the wall of eye to allow fluid from the inside of the eye to flow out of the...
- Written by InnovativEyes

What’s up with people wearing those big sunglasses after cataract surgery?
The main reason is for protection - physical protection to assure nothing hits the eye immediately after surgery, and protection from sunlight and other bright lights.
We...




